Home Advocacy Policy Issues State & Federal Issues
State & Federal Issues
KHA monitors federal issues affecting Kentucky hospitals, including issues related to Medicaid, COVID-19, price transparency, and surprise billing laws surrounding out-of-network billing.
KHA Members:
- Login to review all comments submitted by KHA on various issues
- KHA hosts a forum for hospitals to meet with Medicaid managed care organizations (MCOs) on a monthly basis to discuss ongoing issues. Login to access issue logs and recordings of each meeting.
State Policy Papers
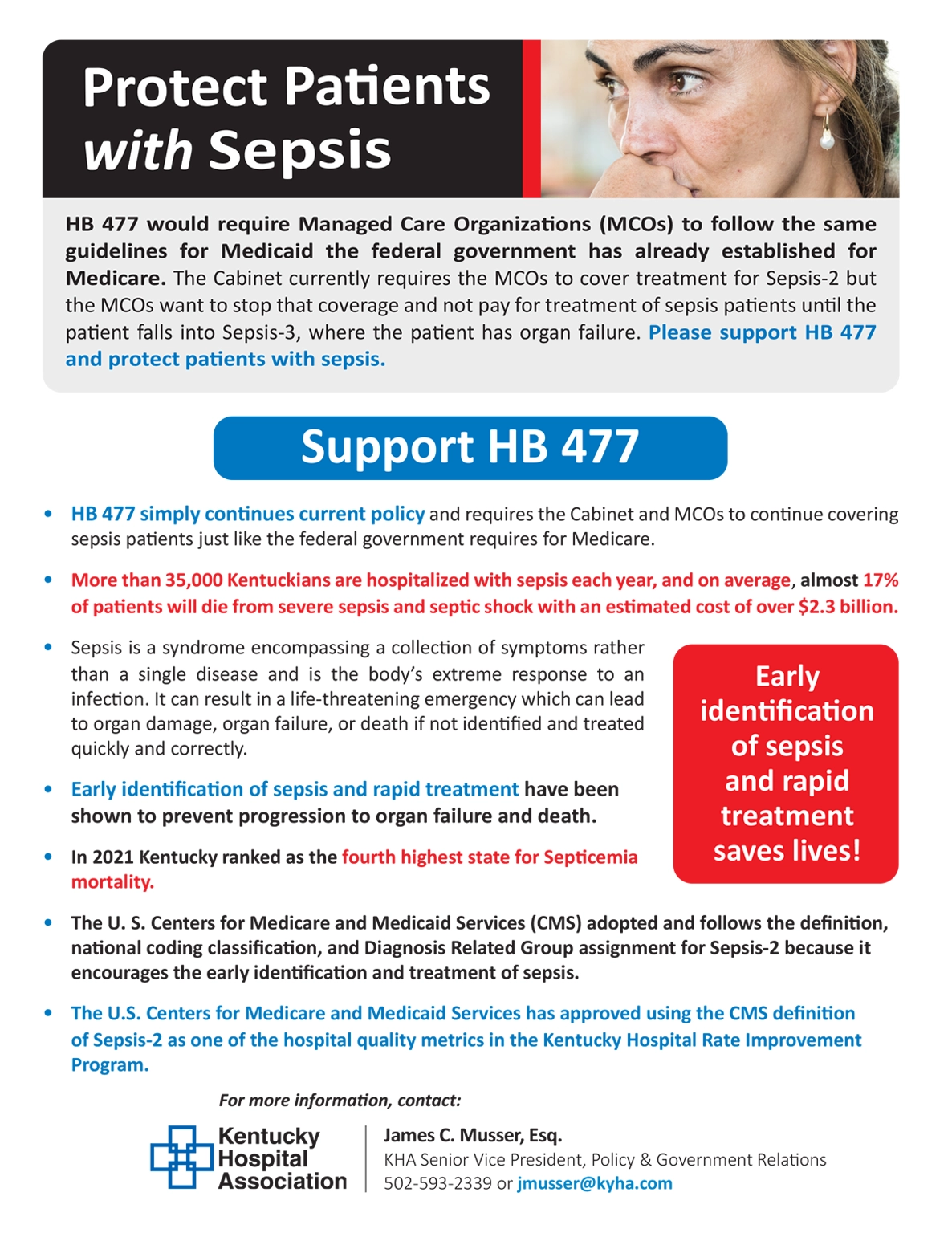
Protect Patients with Sepsis
HB 477 would require Managed Care Organizations (MCOs) to follow the same guidelines for Medicaid the federal government has already established for Medicare. (2024)
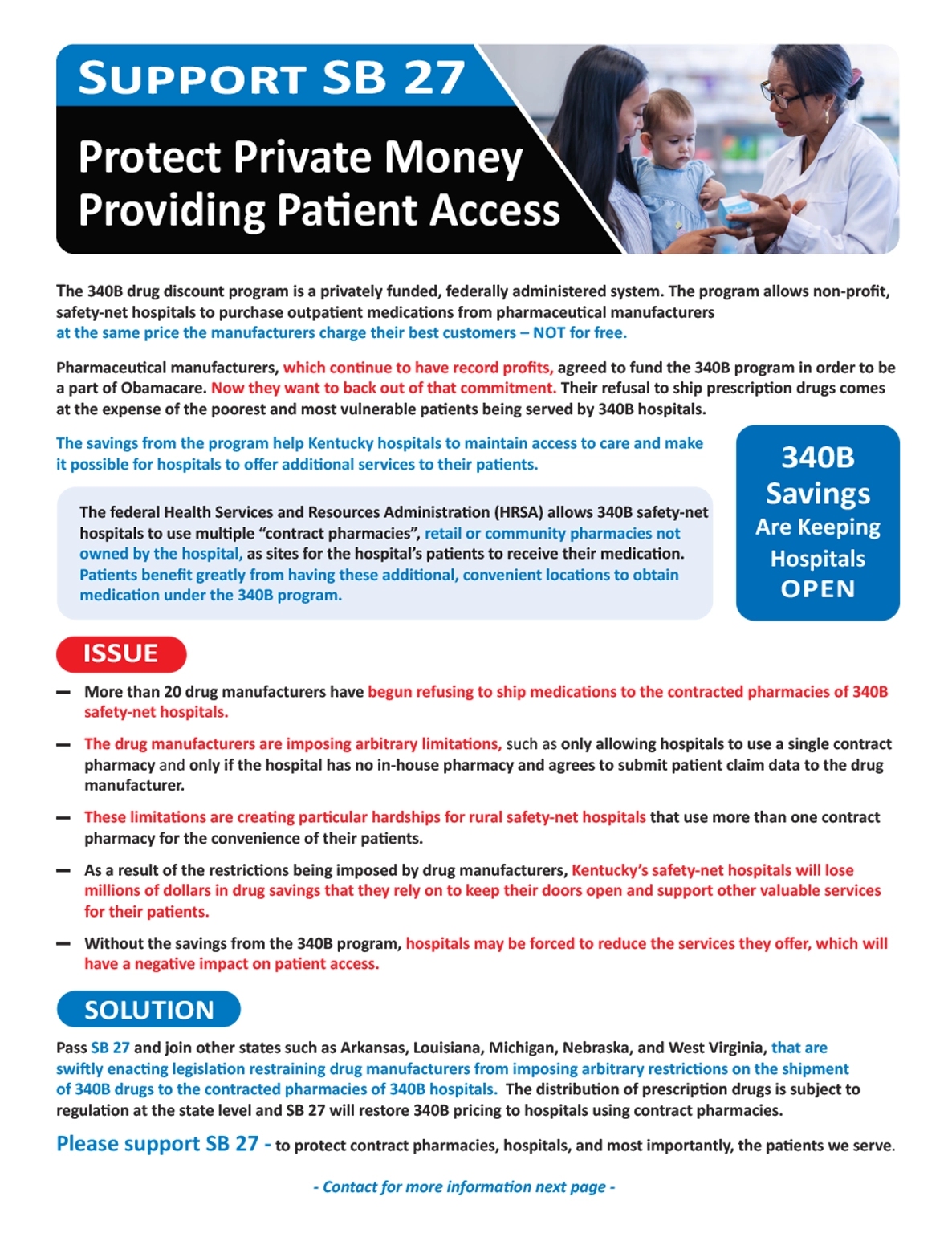
Support SB 27: Protect Private Money Providing Patient Access
Please support SB 27 – to protect contract pharmacies, hospitals, and most importantly, the patients we serve. (2024)
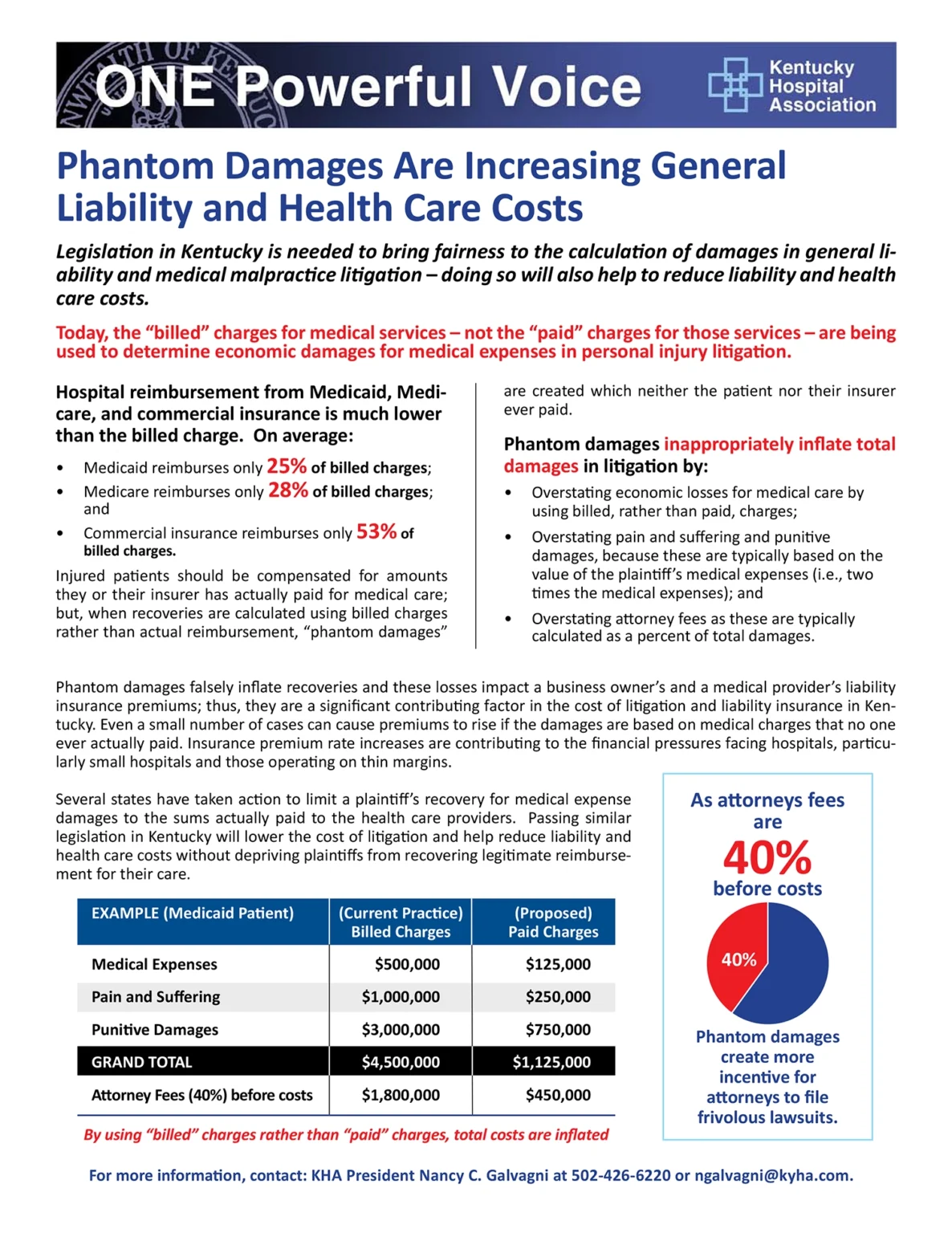
Phantom Damages
Legislation in Kentucky is needed to bring fairness to the calculation of damages in general liability and medical malpractice litigation – doing so will also help to reduce liability and health care costs. (2020)
Federal Policy Papers
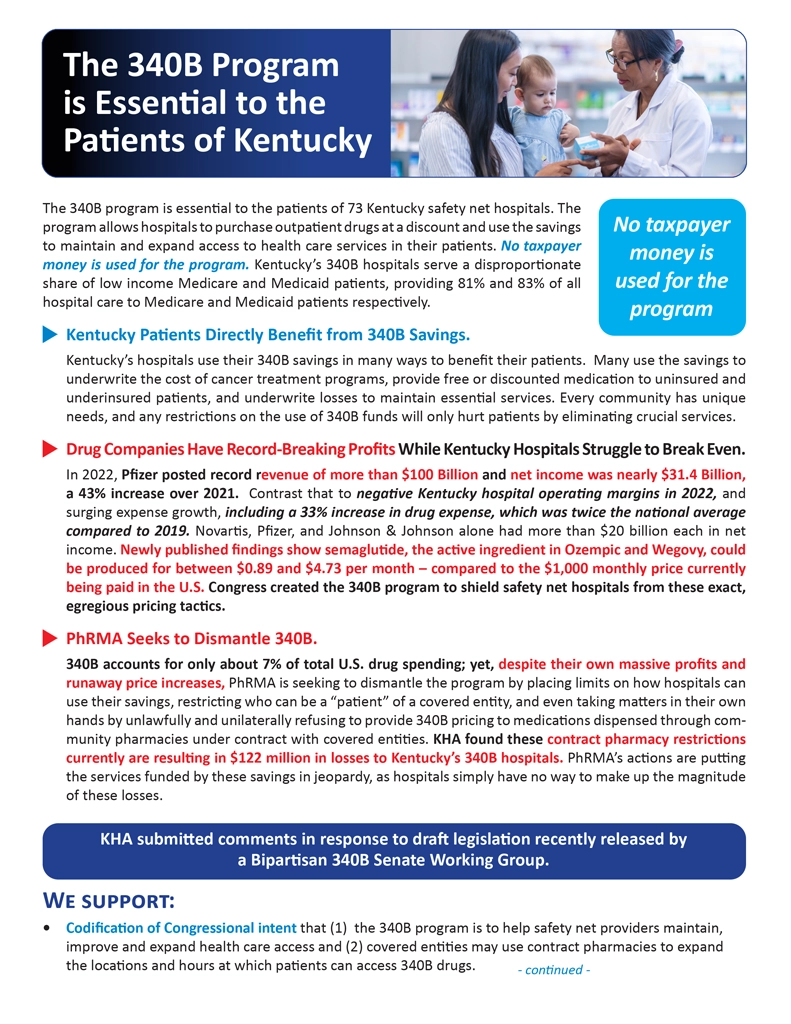
The 340B Program Is Essential to the
Patients of Kentucky
The 340B program is essential to the patients of 73 Kentucky safety net hospitals. (2024)
340B Fact Sheet
The 340B program allows hospitals to purchase outpatient drugs at a discount and use the savings to maintain and expand access to health care services in their patients.(2024)
Federal Surprise Billing Law
The federal “No Surprises Act” was designed to address the concerns surrounding out-of-network billing. (2021)
- Establishing an independent dispute resolution process to determine out-of-network payment amounts between providers (including air ambulance providers) or facilities and health plans.
- Requiring good-faith estimates of medical items or services for uninsured (or self-paying) individuals.
- Establishing a patient-provider dispute resolution process for uninsured (or self-paying) individuals to determine payment amounts due to a provider or facility under certain circumstances.
- Providing a way to appeal certain health plan decisions.
- Overview of rules & fact sheets
- Provider requirements and resources
- Complaint Submission (For providers to submit complaints regarding health plans)
- What to expect when a patient starts payment dispute resolution
- COVID-19 Stimulus Legislation Key Provisions (2021)
- Stop Medicaid DSH Cuts (2020)
- KHA Policy Positions (Summer 2020)
- KHA Policy Positions At-A-Glance (Summer 2020)
- Kentucky Hospitals’ Requests Regarding U.S. House Surprise Billing Legislation (2020)
- Kentucky Hospitals’ Requests Regarding U.S. Senate Surprise Billing Legislation (2020)
- COVID-19 Federal Relief for Kentucky’s Hospitals (2020)
- Kentucky Hospitals Support Medicaid DSH Reform (2020)
- Kentucky Hospitals Support Medicare Payment Adequacy (2018)
- Price Transparency
